Spinal discs play a crucial role in the lower back, serving as shock absorbers between the vertebrae, supporting the upper body, and allowing a wide range of movement in all directions.
If a disc herniates and leaks some of its inner material, though, the disc can quickly go from easing daily life to aggravating a nerve, triggering back pain and possibly pain and nerve symptoms down the leg.
Lumbar herniated disc most often affects people aged 35 to 50.
Disc herniation symptoms usually start for no apparent reason. Or they may occur when a person lifts something heavy and/or twists the lower back, motions that put added stress on the discs.
Lumbar herniated discs are a widespread medical problem, most often affecting people age 35 to 50.
This article covers how a lumbar herniated disc develops, how it is diagnosed, and the available surgical and non-surgical treatment options.
How a Lumbar Disc Herniates
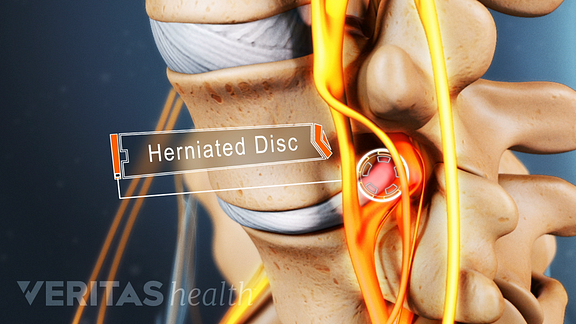
A tough outer ring called the annulus protects the gel-like interior of each disc, known as the nucleus pulposus.
Due to aging and general wear and tear, the discs lose some of the fluid that makes them pliable and spongy. As a result, the discs tend to become flatter and harder. This process—known as disc degeneration—starts fairly early in life, often showing up in imaging tests in early adulthood.
When pressure or stress is placed on the spine, the disc’s outer ring may bulge, crack, or tear. If this occurs in the lower back (the lumbar spine), the disc protrusion may push against the nearby spinal nerve root. Or the inflammatory material from the interior may irritate the nerve. The result is shooting pains into the buttock and down the leg.
See Lumbar Radiculopathy
A person with a herniated disc may be told by the doctor that degenerative disc disease led to the lumbar herniated disc. This term can be alarming and misleading. Degenerative disc disease is not a progressive disease per se, and it does not always cause chronic or persistent problems.
Lumbar Radiculopathy
Radicular pain is often secondary to compression or inflammation of a spinal nerve. When the pain radiates down the back of the leg to the calf or foot, it would in lay terms be described as sciatica. This type of pain is often deep and steady, and can usually be reproduced with certain activities and positions, such as sitting or walking.
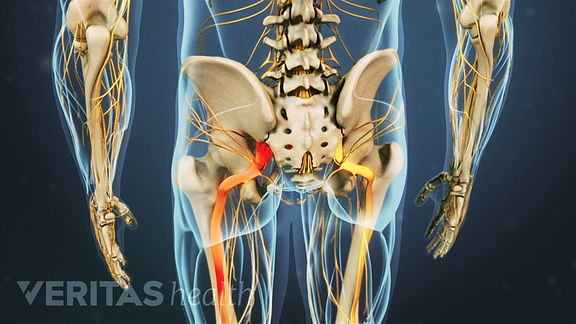
The pain usually follows the involved dermatome in the leg – the area of distribution of the leg covered by the specific nerve. When a nerve at the L4-5 or L5-S1 level is affected (bottom two levels), this dermatome is usually the sciatic nerve, which runs down the back of each leg to the foot.
Radicular pain may also be accompanied by numbness and tingling, muscle weakness and loss of specific reflexes. When actual nerve dysfunction is noted (prior noted symptoms), this is termed “radiculopathy”.
Area of Pain Distribution
Radicular pain radiates into the lower extremity (thigh, calf, and occasionally the foot) directly along the course of a specific spinal nerve root. The most common symptom of radicular pain is sciatica (pain that radiates along the sciatic nerve – down the back of the thigh and calf into the foot). Sciatica is one of the most common forms of pain caused by compression of a spinal nerve in the low back. It often will be caused by compression of the lower spinal nerve roots (L5 and S1).
With this condition, the leg pain is typically much worse than the low back pain, and the specific areas of the leg and/or foot that are affected depends on which nerve in the low back is affected. Compression of higher lumbar nerve roots such as L2, L3 and L4 can cause radicular pain into the front of the thigh and the shin.
Diagnosis of Lumbar Radiculopathy
A radiculopathy is caused by compression, inflammation and/or injury to a spinal nerve root in the low back. Causes of this type of pain, in the order of prevalence, include:
- Herniated disc with nerve compression – by far the most common cause of radiculopathy
- Foraminal stenosis (narrowing of the hole through which the spinal nerve exits due to bone spurs or arthritis) – more common in elderly adults
- Diabetes
- Nerve root injuries
- Scar tissue from previous spinal surgery that is affecting the nerve root
Sciatica, the term commonly used to describe radicular pain along the sciatic nerve, describes where the pain is felt but is not an actual diagnosis. The clinical diagnosis is usually arrived at through a combination of the patient’s history (including a description of the pain) and a physical exam. Imaging studies (MRI, CT-myelogram) are used to confirm the diagnosis and will typically show the impingement on the nerve root.