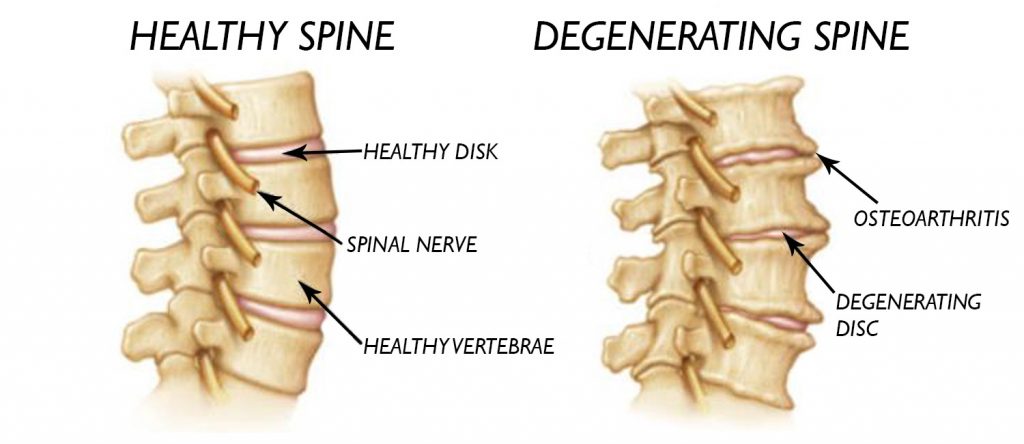
Degenerative disc disease is a condition that is commonly misunderstood. A degenerated disc is not actually a disease—it is part of the normal aging of the spine. When a spinal disc degenerates, it loses its ability to function efficiently as part of the spinal joint, which in turn can lead to back pain and possibly pain that radiates through the extremities.
A degenerating spinal disc does not always lead to pain or other symptoms. Because the disc itself has very little innervation, pain usually occurs when the degenerating disc affects other structures in the spine (such as muscles, joint, or nerve roots).
Pain associated with degenerative disc disease generally stems from two main factors:
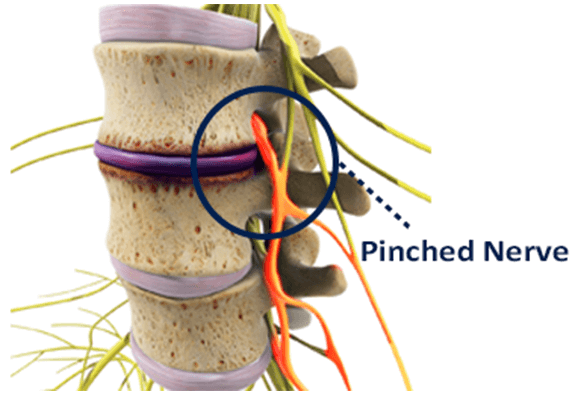
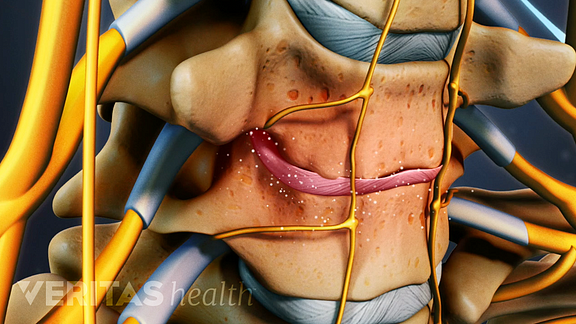
- Inflammation. Inflammatory proteins from the disc space interior can leak out as the disc degenerates, causing swelling in the surrounding spinal structures. This inflammation can produce muscle tension, muscle spasms, and local tenderness in the back or neck. If a nerve root becomes inflamed, pain and numbness may radiate into the arm and shoulder (called a cervical radiculopathy in cases of cervical disc degeneration), or into the hips or leg (called a lumbar radiculopathy, in cases of lumbar disc degeneration).
- Abnormal micro-motion instability. The cushioning and support a disc typically provides decreases as the disc’s outer layer (the annulus fibrosis) degenerates, leading to small, unnatural motions between vertebrae. These micro-motions can cause tension and irritation in the surrounding muscles, joints, and/or nerve roots as the spinal segment becomes progressively more unstable, causing intermittent episodes of more intense pain.
Both inflammation and micro-motion instability can cause lower back or neck muscle spasms. The muscle spasm is the body’s attempt to stabilize the spine. Muscle tension and spasms can be quite painful, and are thought to cause the flare-ups of intense pain associated with degenerative disc disease.
What Happens in The Spine During Disc Degeneration?
Degenerative disc disease primarily concerns a spinal disc, but will most likely impact other parts of the spine as well. The two findings most correlated with a painful disc are:
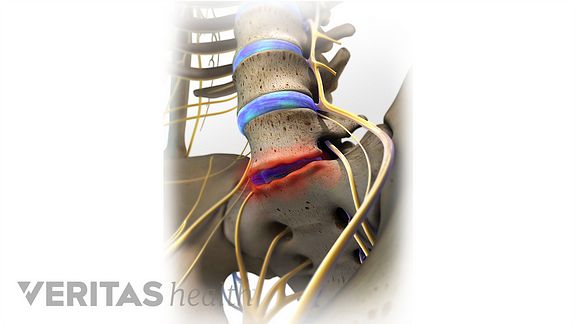
- Cartilaginous Endplate Erosion. Like other joints in the body, each vertebral segment is a joint that has cartilage in it. In between a spinal disc and each vertebral body is a layer of cartilage known as the endplate. The endplate sandwiches the spinal disc and acts as a gatekeeper for oxygen and nutrients entering and leaving the disc. As the disc wears down and the endplate begins to erode, this flow of nutrition is compromised, which can hasten disc degeneration. As the disc goes through this process, the disc space will collapse.
- Disc space collapse. As a disc degenerates the disc space will collapse, placing undue strain on the surrounding muscles as they support the spine and shortening the space between vertebrae, leading to additional micro-motion and spinal instability.
These processes typically progress gradually rather than all at once. Endplate erosion and disc space collapse can add to spinal instability, tension in the surrounding muscles, and both local and nerve root pain.
Causes and Risk Factors of Lumbar Degenerative Disc Disease
Pain from degenerative disc disease is typically caused by strain on the muscles supporting the spine and inflammation around the disc space.
Degeneration occurs because of age-related wear-and-tear on a spinal disc, and may be accelerated by injury, health and lifestyle factors, and possibly by genetic predisposition to joint pain or musculoskeletal disorders. Degenerative disc disease rarely starts from a major trauma such as a car accident. It is most likely due to a low-energy injury to the disc.
Lumbar Degenerative Disc Disease Causes
The low back pain associated with lumbar degenerative disc disease is usually generated from one or both of following sources:
- Inflammation, as the proteins in the disc space irritate the surrounding nerves—both the small nerve within the disc space and potentially the larger nerves that go to the legs (the sciatic nerve).
- Abnormal micro-motion instability, when the outer rings of the disc, called the annulus fibrosis, are worn down and cannot absorb stress on the spine effectively, resulting in movement along the vertebral segment.
Over a long period of time the pain from lumbar degenerative disc disease eventually decreases, rather than becoming progressively worse. This pain relief occurs because a fully degenerated disc no longer has any inflammatory proteins (that can cause pain) and usually collapses into a stable position, eliminating the micro-motion that generates the pain.
The Degenerative Cascade
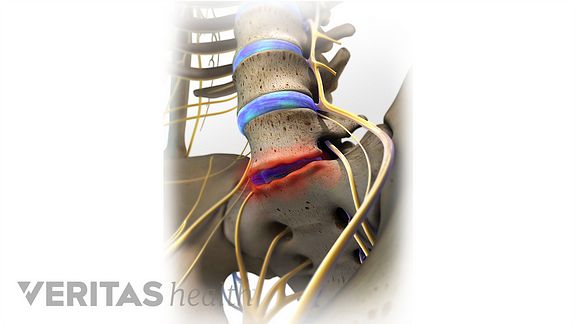
When a disc endplate is damaged, the blood supply to the discs is compromised, leading to a lack of nutrients and oxygen that are essential for restoring damaged tissues. Once one stress or injury occurs, a disc can begin to wear down relatively quickly in a process called the degenerative cascade.
The degenerative cascade is a slow process that typically continues for 10 to 30 years and usually consists of the following cycle:
- An initial stress or injury may occur, causing acute pain that may be severe. Stiffness and limited mobility may occur immediately after the initial injury or stress to the disc. In many cases, there is no clear injury that causes the onset of symptoms.
- The affected spinal segment then undergoes a long period of relative instability. As the disc height decreases, the muscles, ligaments, and facet joints around the disc space gradually adjust to stabilize the spine again. During this phase, there are periodic flare-ups of moderate or intense low back pain.
- Once the spinal segment stabilizes, pain and other symptoms tend to alleviate.
Risk Factors for Degenerative Disc Disease
Lifestyle factors that affect overall health can have an impact on the spinal discs. Risk factors for degenerative disc disease include:
- Family history of back pain or musculoskeletal disorders
- Excessive strain on the low back caused by sports, frequent heavy lifting, or labor-intensive jobs
- Strain on the lumbar spinal discs due to prolonged sitting and/or poor posture
- Lack of support for the discs due to weak core muscles
- Obesity
- Smoking, or any form of nicotine intake
Disc degeneration is a common part of aging, but not all people develop pain or any remarkable symptoms. Symptoms tend to arise when spinal instability, muscle tension, and possibly nerve root irritation occurs.
Cervical Degenerative Disc Disease
Cervical degenerative disc disease is a common cause of neck pain and radiating arm pain. It develops when one or more of the cushioning discs in the cervical spine starts to break down due to wear and tear.
There may be a genetic component that predisposes some people to more rapid wear. Injury may also accelerate and sometimes cause the development of the degenerative changes.
How Cervical Discs Can Degenerate
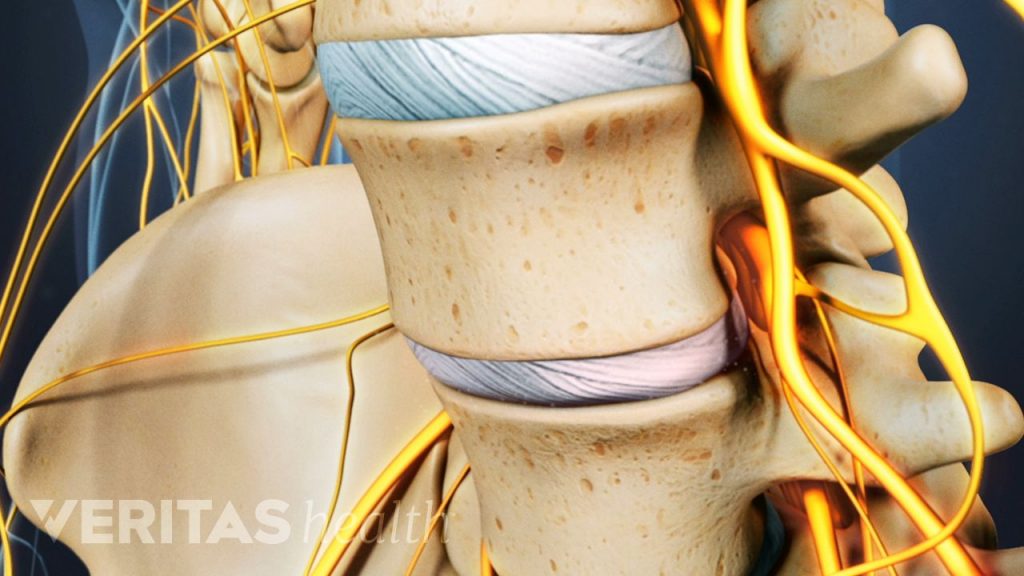
Normally, there are six gel-like cervical discs (one between each of the cervical spine’s vertebrae) that absorb shock and prevent vertebral bones from rubbing against each other while the neck moves.
Each disc is comprised of a tough but flexible outer layer of woven cartilage strands, called the annulus fibrosus. Sealed inside the annulus fibrosus is a soft interior filled with a mucoprotein gel called the nucleus pulposus. The nucleus gives the disc its shock absorption property.
In children, the discs are about 85% water. The discs begin to naturally lose hydration during the aging process. Some estimates have the disc’s water content typically falling to 70% by age 70,1 but in some people the disc can lose hydration much more quickly.
As the disc loses hydration, it offers less cushioning and becomes more prone to cracks and tears. The disc is not able to truly repair itself because it does not have a direct blood supply (instead getting nutrients and metabolites via diffusion with adjacent vertebrae through the cartilaginous endplates). As such, a tear in the disc either will not heal or will develop weaker scar tissue that has potential to break again.
Treatment for Degenerative Disc Disease Video
Degenerative disc disease is frequently the cause of low back pain, especially in young adults.
Although this condition can cause lower back pain symptoms over a long period of time, the good news is that the pain is usually manageable with various conservative treatment options (meaning back care that doesn’t involve surgery).
Low Back Pain and Degenerative Disc Disease Treatment Goals
The vast majority of people with degenerative disc disease experience low back pain symptoms that flare up periodically, but don’t get worse over time. For those people, the main goals for managing lower back pain caused by degenerative disc disease are usually:
- Achieving enough pain relief to be able to engage in lower back pain exercises and a rehabilitation program
- Preventing the application of excess stress on the disc through proper ergonomics and posture
- Trying to manage the low back pain and maintaining an ability to function enough at home and at work.
advertisement
Degen. Disc Disease Info:
Disc Disease Symptoms
Lumbar Disc Disease
Cervical Disc Disease
Most types of surgery for ongoing, debilitating pain and loss of function from degenerative disc disease are fairly extensive, so it is usually in the best interest of most patients to manage their low back pain using non-surgical approaches and self-care. Over time, the low back pain and other symptoms of degenerative disc disease will usually subside. This happens because the disc starts to become stiffer with age, and a stiffer disc stabilizes the motion segment and thus reduces pain. However, this is a very slow process that occurs over many years.
Lower Back Pain Treatment for Degenerative Disc Disease
Pain from degenerative disc disease is caused by a combination of instability at the motion segment and inflammation from the degenerated discs. Both the instability and the inflammation have to be addressed for the back pain treatment to be effective.
The treatments for degenerative disc disease are either passive (done to the patient) or active (done by the patient). Usually a combination of treatments is used to help control the symptoms. Passive treatments are rarely effective on their own—some active component, such as exercise, is almost always required.
Spinal Pain Treatment for Degenerative Disc Disease
Passive treatments for low back pain from degenerative disc disease may include:
- Pain medication. Typical pain medications used to treat the low back pain include acetaminophen, NSAIDs, oral steroids, narcotic drugs, and muscle relaxants. Each type of medication has strengths, limitations, and risks, and the patient’s particular low back problem and overall health will determine which pain reliever, if any, is indicated.
- Chiropractic manipulation. Manual manipulation by a chiropractor or other qualified health professional is thought to provide lower back pain relief by taking pressure off sensitive neurological tissue, increasing range of motion, restoring blood flow, reducing muscle tension, and creating a series of chemical reactions in the body (such as endorphin release) that act as natural painkillers.See Chiropractic Treatments for Lower Back Pain
- Epidural injections. An epidural injection into the spine delivers steroids that can provide low back pain relief by decreasing inflammation in the painful area.